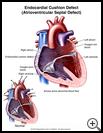
Endocardial Cushion Defect
(Atrioventricular Septal Defect)
What is an endocardial cushion defect?
Endocardial cushion defect is a birth defect of the heart. It is also called atrioventricular canal defect or atrioventricular septal defect (AVSD). AVSD involves problems with the structure of the heart. The heart normally has 2 upper chambers (atria) and 2 lower chambers (ventricles). A normal heart also has 2 heart valves that separate the upper and lower chambers (the tricuspid and mitral valves).
In AVSD, there may be a large hole in the wall between the chambers of the heart (the atrioventricular septum). In some cases the tricuspid and mitral valves may not be separate. Instead, there can be one large valve between the upper and lower chambers of the heart (called the common atrioventricular valve).
The large opening in the center of the heart allows oxygen-rich and oxygen-poor blood to mix. The heart pumps blood in a way that is not efficient. The heart has to work harder and it becomes enlarged.
How does it occur?
AVSD can happen when the heart does not develop normally before birth. The cause is not known, but it is commonly found in babies with Down syndrome.
What are the symptoms?
The symptoms may start at any time from birth to several months after birth. Most babies with this problem do not eat well. They may not grow normally. They breathe fast. They often have colds and may get pneumonia. They may sweat and be clammy.
How is it diagnosed?
Children with AVSD usually have a heart murmur, which a healthcare provider can hear with a stethoscope. A heart murmur is an extra sound made between heartbeats. These murmurs are caused by the blood flowing abnormally through the heart.
To diagnose the problem, the following tests may be done:
- a chest X-ray to look for enlargement of the heart
- an electrocardiogram (EKG), which is a recording of the electrical activity of the heart
- an echocardiogram, which uses sound waves to make pictures of the heart
- heart catheterization, which is a procedure for passing a small tube through an artery of the leg and into the heart to take special X-ray pictures of the heart with a dye.
How is it treated?
If your baby has symptoms, medicines will be given to help your baby feel better and get strong enough to have surgery. Medicines that may be used include:
- ACE inhibitors or angiotensin-receptor blockers (ARBs) help decrease the work load on the heart.
- Digoxin helps strengthen the heart muscle.
- Diuretics (water pills) help remove excess fluid from the body so the heart doesn't have to work as hard.
- Antibiotics may be given if your child has an infection.
Surgery is needed to repair the defect. The surgeon will close the hole in the septum and rebuild the valves if needed.
In rare cases, the defect is too complex to make all the repairs at one time. The surgeon may place a band around the lung artery to narrow the artery and reduce blood flow to the lungs. Then the heart will not have to work as hard, and the lungs will be protected from high blood pressure. When the child is older, the pulmonary artery band can be removed and corrective surgery done.
How long will the effects last?
If a child with AVSD is not treated, they may:
- Often have pneumonia.
- Have an enlarged heart, which means the heart won’t pump as well as it should.
- Have high blood pressure in the lungs.
- Have heart failure, which means the heart is not pumping as well as it should.
With treatment, a child has a much better chance for a healthier life. Sometimes, the heart valves are too small or the valves allow blood to leak backward. If the valves do not work properly after surgery, the child may need another surgery to fix them. A child may also have damage to the lungs that makes it harder to breathe, or they may have abnormal heart rhythms.
Your child will need to have regular follow-up visits with a heart specialist.
Ask your healthcare provider if your child should take antibiotics to prevent infection before having dental work or procedures that involve the rectum, bladder, or vagina.
Last modified: 2011-05-26
Last reviewed: 2011-05-19